What Is CareConnections®?
CareConnections® is a web-based suite of rehabilitation medical management services. It is the only complete outcome improvement system that uses combinations of tools to assist providers and payers with the medical management of patients and clinical services.
CareConnections® takes two ingredients – patient outcome data and clinical practice guidelines – and uses them as a part of an automated care management process. The CareConnections® website provides a platform for the registration of an individual patient’s information and processes an immediate automated Registration Summary. The Registration Summary provides valuable, instantly delivered information that guides care and signals when updated clinical metrics are required.
CareConnections® is a single system, serving the needs of all stakeholders to eliminate inefficiency and 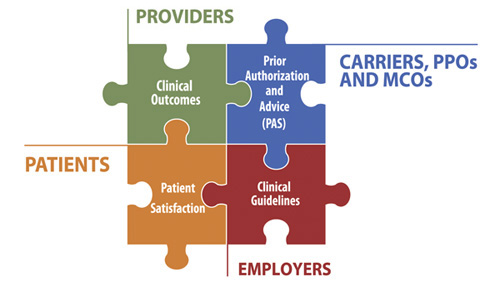 the frustration that drives up administrative costs and steals from the value of patient care. It’s the practical way to promote clinical integration and administrative cost sharing across the health care system.
the frustration that drives up administrative costs and steals from the value of patient care. It’s the practical way to promote clinical integration and administrative cost sharing across the health care system.
CareConnections® has four main parts:
- Clinical Practice Guidelines
- Outcome Measurement System
- Patient Satisfaction Feedback System
- Prior Authorization/Advice System (PAS)
What can CareConnections® be used for?
- UM/QM – Utilization and Quality Management – Mentoring – and Proving VALUE
- Each part can be used by individual clinics, group practices or networks to promote high quality care and effective utilization of services.
- The only system with a combination of practice protocols to guide care, outcomes to measure and monitor effectiveness, a variety of reports to interpret metrics and all packaged in a system that can interact with other clinics and payers.
Simply collected, simply understood. Invest in a better outcome!
Call 1-800-821-9319 for more information
![]()
Clinical Practice Guidelines
Easily understood patterns of practice per diagnosis to guide care using appropriate evaluation and treatment techniques.
- Over 100 individual guidelines, 20 new protocols in 2014
- Promotes evidence-based care
- Reduces variation in treatment
- Mentors staff
- Referral source marketing aids
Outcome Measurement System
A simple to understand questionnaire to measure patient progress, easy to use web portal for data entry and report retrieval.
- Easily collect – Functional Index, Perceived Pain, Acuity and Work Status data metrics on paper or electronic kiosk
- Use for Medicare Functional Impairment and PQRS compliance
- Questions help set functional goals
- Over 400+ easy to interpret Outcome Reports
Patient Satisfaction Feedback System
An easy to understand patient survey about their clinical experience.
- Easily collect feedback on patient experience
- Monitor/manage patient’s experience to improve customer satisfaction
- Collect patient feedback to rate health plans
- Promote your practice to referral sources and payers
Prior Authorization/Advice System (PAS)
Interactive platform for internal UM management or for use by groups and networks to interface with payers.
- Manage your clinician’s utilization profile
- System to engage payers in preferential or exclusive contracts
- Manage risk-contract utilization across clinics
- Generate network administrative revenues
Call 1-800-821-9319 for more information